What Are Kidney Cysts?
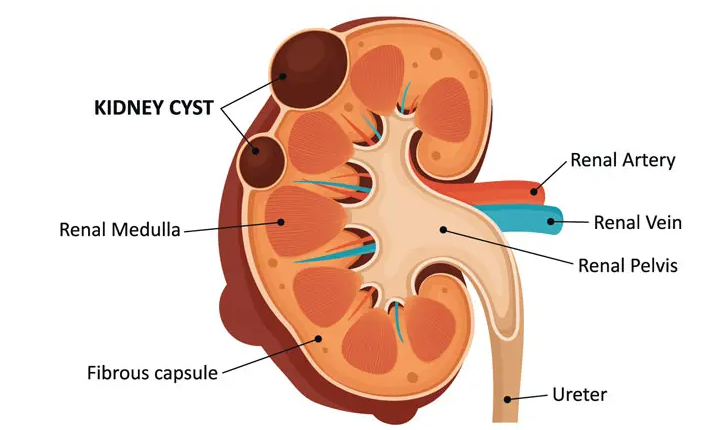
Kidney cysts are round or oval formations filled with clear fluid that can appear on one or both kidneys, either singly or in greater numbers.
For single cysts, the exact cause is unknown, but it is believed to be related to blocked renal tubules. However, when there are multiple cystic formations present in both kidneys, this condition is often associated with adult polycystic kidney disease or medullary cystic disease (juvenile nephronophthisis). In these cases, the primary factor is genetic inheritance or, more rarely, spontaneous genetic mutations. Polycystic kidney disease (PKD) is a serious condition that often leads to end-stage kidney failure, requiring dialysis or kidney transplantation. Patients with PKD may also develop cysts on other organs (e.g., liver, pancreas, ovaries) and have associated organ anomalies.
Simple (Dysontogenetic) Cysts
Simple cysts are round, well-defined, anechoic masses located in or on the kidney, with a clear acoustic enhancement visible on ultrasound. They can be confidently identified as primary (dysontogenetic) cysts if they show no vascularization on color Doppler examination and if there are no other structural abnormalities in the kidney. Whether single or multiple, these cysts are generally tubular retention cysts, originating from dilation of the Bowman’s capsule or proximal tubules. As a result, they have a cyst wall that produces typical ultrasound entry or exit echoes, though they may not always be directly visible. Primary dysontogenetic cysts also have a typical location within the kidney.
Multiple Dysontogenetic Cysts
Kidneys containing multiple cysts are generally of normal size, unlike polycystic kidneys. In polycystic kidneys, the renal cortex, medullary pyramids, and renal sinus are well-defined, whereas polycystic kidneys have indistinct borders and are greatly enlarged with numerous cysts.
Polycystic Kidneys (Dysontogenetic)
This condition includes the polycystic malformation of distal renal tubules, tubular epithelium, or tubular walls, leading to a predominantly bilateral polycystic transformation of the kidneys. In ultrasound images, these kidneys appear significantly enlarged with numerous cysts that alter the contours of the renal capsule, causing indistinct kidney borders. There is variable parenchymal reduction due to cyst compression, the “blooming” effect, and interstitial fibrosis.
Polycystic kidneys are commonly associated with cysts in the liver and other organs, and initial ultrasound findings are unmistakable.
Atypical or Secondary Cysts
Atypical or secondary cysts differ from simple, uncomplicated cysts in their shape, location, or contents. They can be ellipsoid, polygonal, or clustered, may have parapelvic or extrarenal locations, and may contain internal echoes (thickened walls, septa, sediment, or blood clots) as well as blood vessels in malignant tumors.
Septated Cysts
Kidney cysts may sometimes have thin septa dividing them into separate compartments. These septated cysts require careful evaluation on ultrasound to differentiate from cystic renal cell carcinoma. Such lesions require monitoring and possible surgery. Differential diagnosis should include dehydrated cysts and, in young boys, multilocular cystic nephroma (benign cystic nephroma), which presents on ultrasound as a complex kidney mass with numerous anechoic cysts separated by echogenic septa.
Retention Cysts Due to Scarring
Secondary retention cysts occur in one-third to one-half of patients with chronic interstitial nephritis who require dialysis. These cysts are the result of scarring in the renal tubules, and most are deformed, very small, and generally located in the renal cortex.
Hydrated Cyst and Echinococcal (Tapeworm) Infection
Infections from Echinococcus granulosus (dog tapeworm), which forms primary cysts with internal daughter cysts, and Echinococcus multilocularis (fox tapeworm), where daughter cysts invade and destroy host tissue from the primary cyst, can cause hydatid disease in humans. The most commonly affected organ is the liver, but other sites, including the kidneys, may also be affected. On ultrasound, these cysts have an echogenic wall, with daughter cysts appearing as a “rosette.” Echinococcus multilocularis may appear as a solid tumor mass. Hydatid cysts require differentiation from cysts with internal septa.
Monitoring and Treatment
When kidney cysts are detected on ultrasound, follow-up monitoring every 6 to 12 months is generally recommended. If there is suspicion of malignant transformation, a CT urogram (CT scan) or optionally, MRI urography, can be conducted. If a tumor change within the cyst is detected, surgical treatment is pursued.